Video
Below is a quick video snap shot of this article.
Definition
Atrial fibrillation is when the atria “twitch” or “quiver” instead of fully contracting.
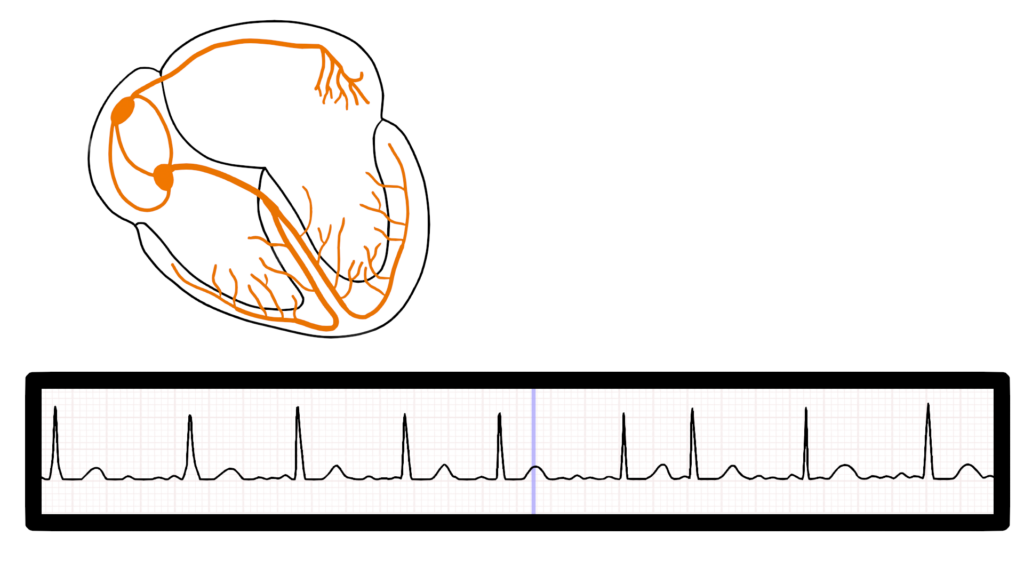
What’s happening in the heart
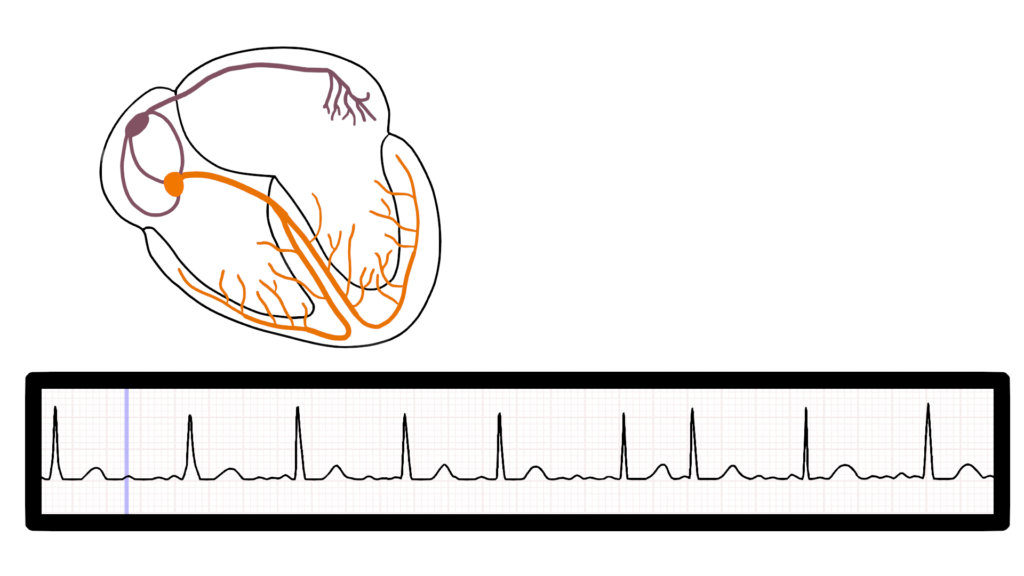
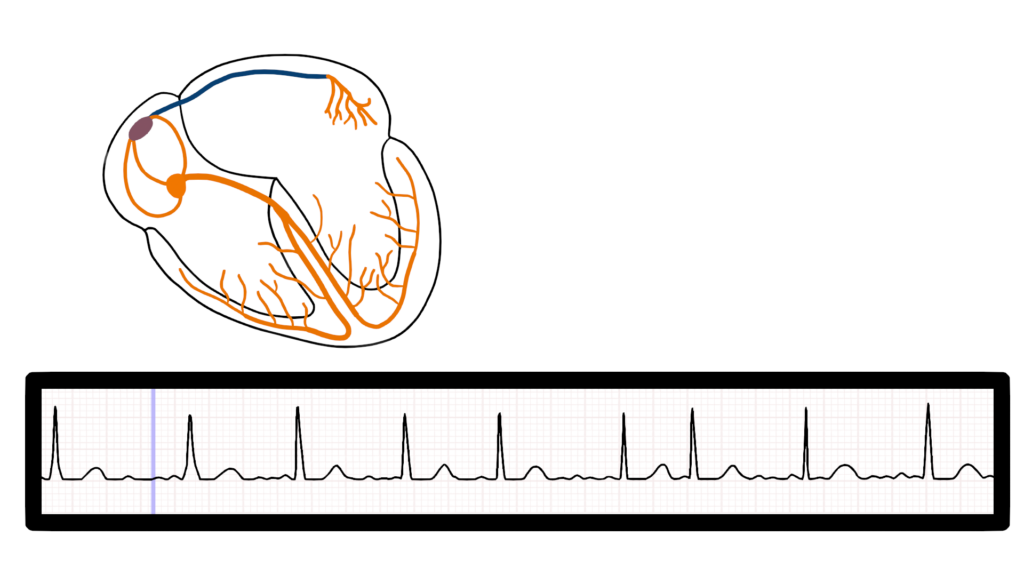
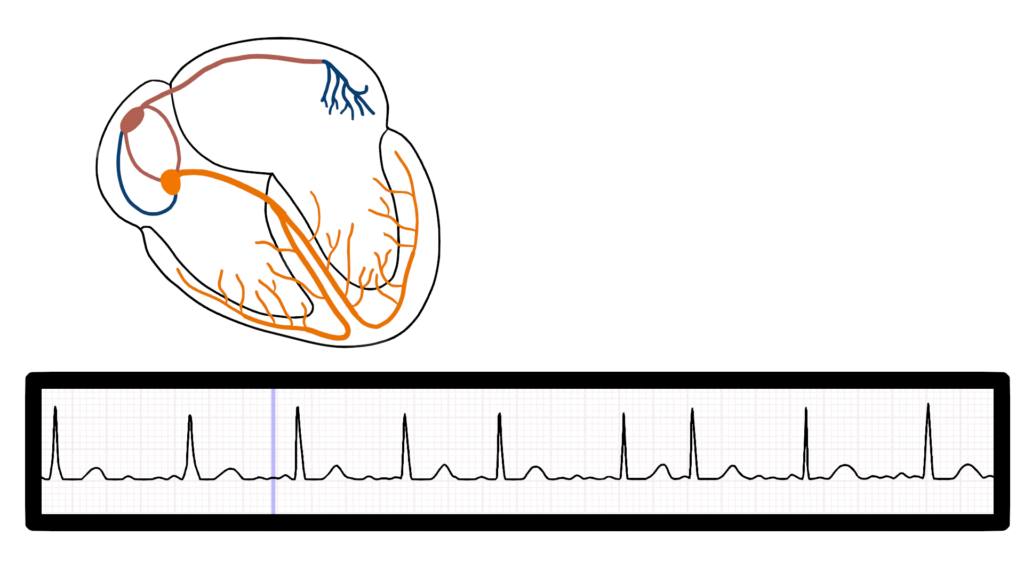
Impulse Origination
First, the impulse originates somewhere within the atria. This may be within the SA or another area of the atrium.
While you can not specifically tell where the impulse started within the atria you will see a variety of P wave shapes based upon the strength and direction of travel of the impulse.
It is important to note that while we may see different types of P waves these do not mean that the atria are actually contracting. Remember the atria only “quiver” as a results of the faulty electrical signals.
Here we can see three different impulse origination’s within the atria.
Ventricular Contraction
At times the impulse will get to the AV and then pass through to the ventricles causing ventricular contraction.
This causes a irregular heart rate due to the erratic nature of impulse flow through the AV node to the ventricles.
Heart rate can vary quite considerably ranging from the normal rate of 60-100 to over 160 depending upon patient condition. See RVR below for more information.
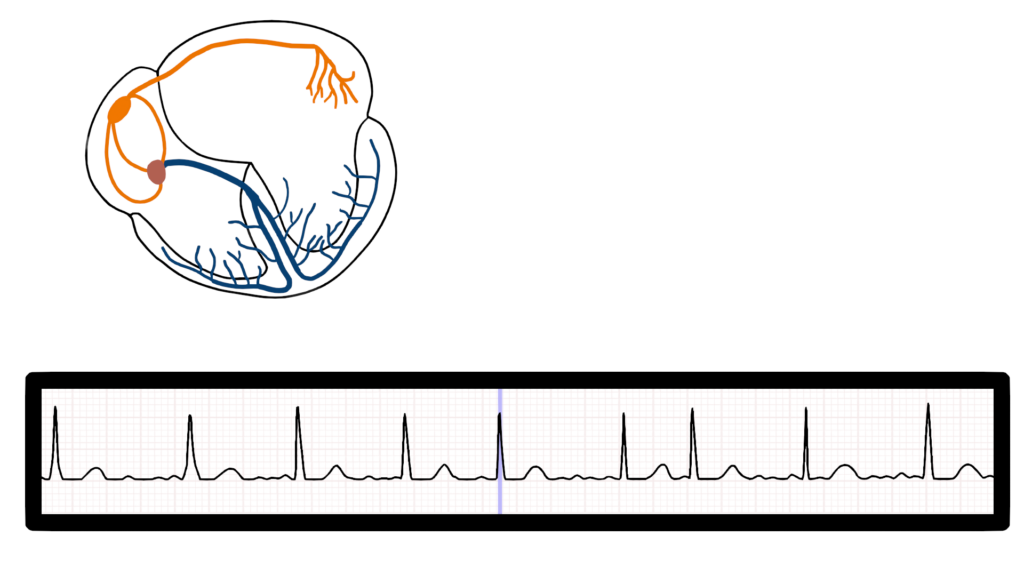
Ventricular Repolarization
Ventricular repolarization will happen as expected following the QRS.
T waves should be present with all QRS complexes.
Seven steps of rhythm interpretation
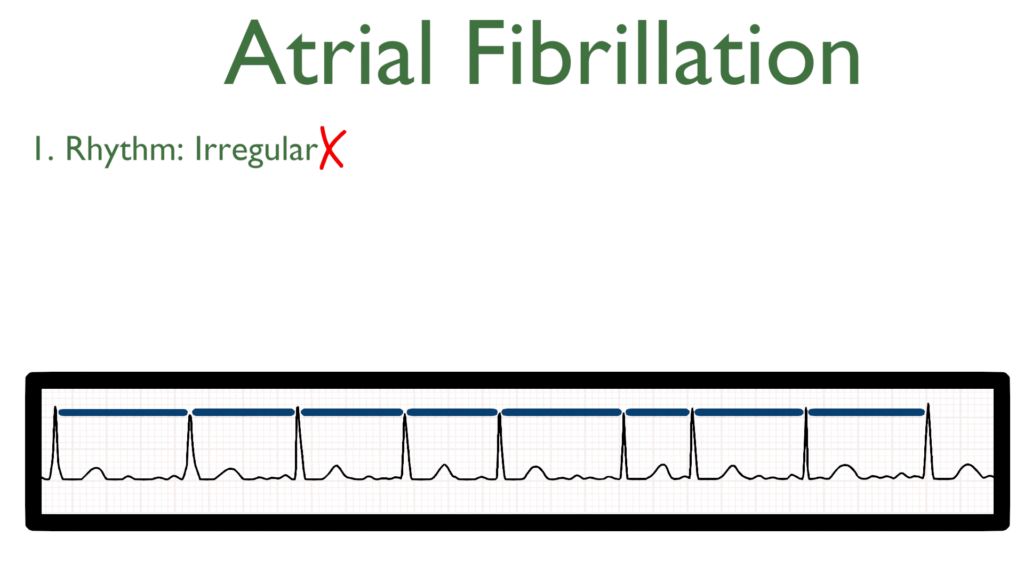
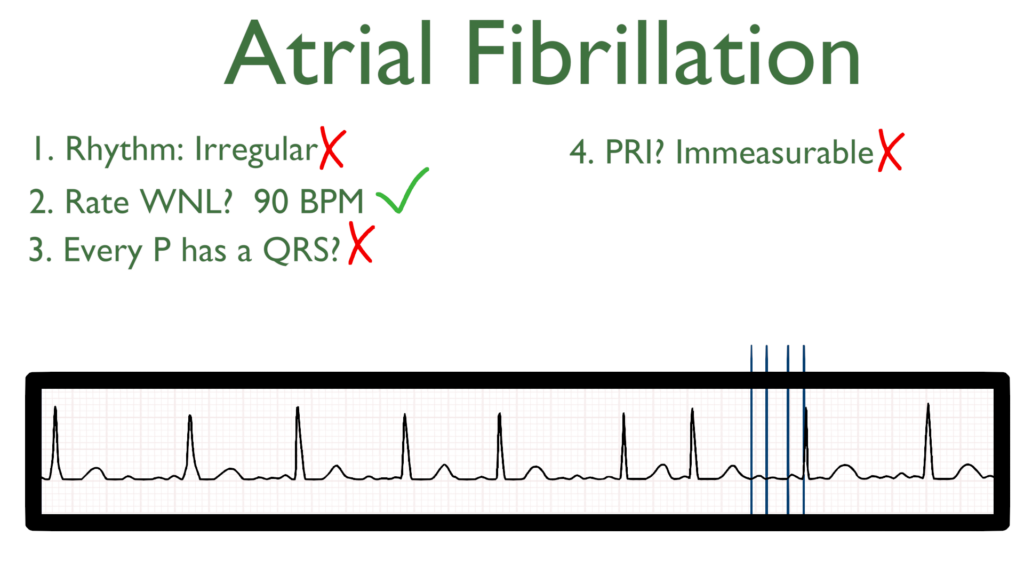
1. Assess the rhythm.
A fib rhythm is often considered irregularly irregular due to erratic impulse flow through the AV node.
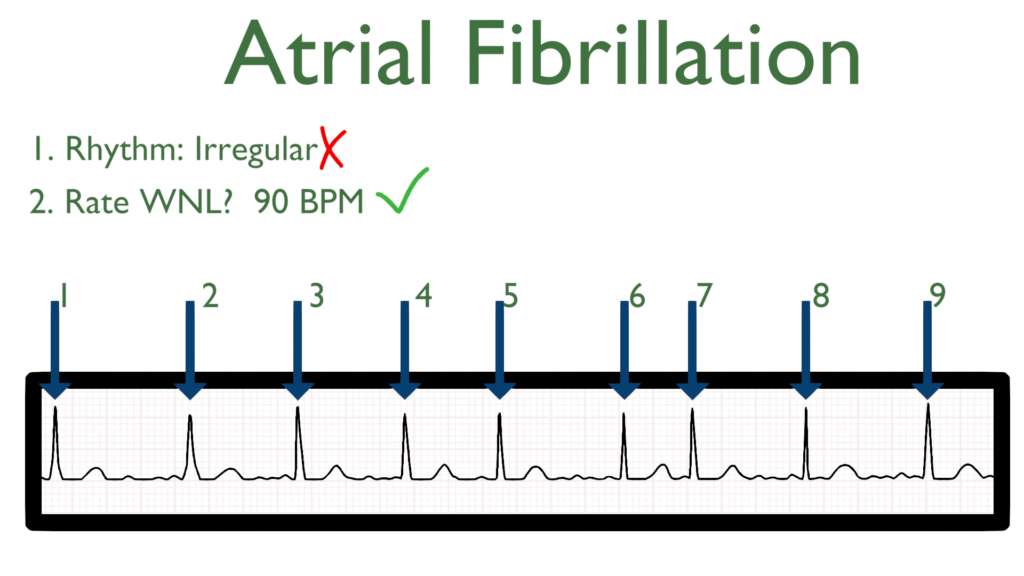
2. Assess the rate.
The rate of A fib will be variable which can generally range anywhere between 60 and 180 bpm.
For more information on why a fib may have an elevated heart rate see Rapid Ventricular Response (RVR) below for more information.
3. Assess atrial and ventricular rates.
P waves will out number the QRS complexes.
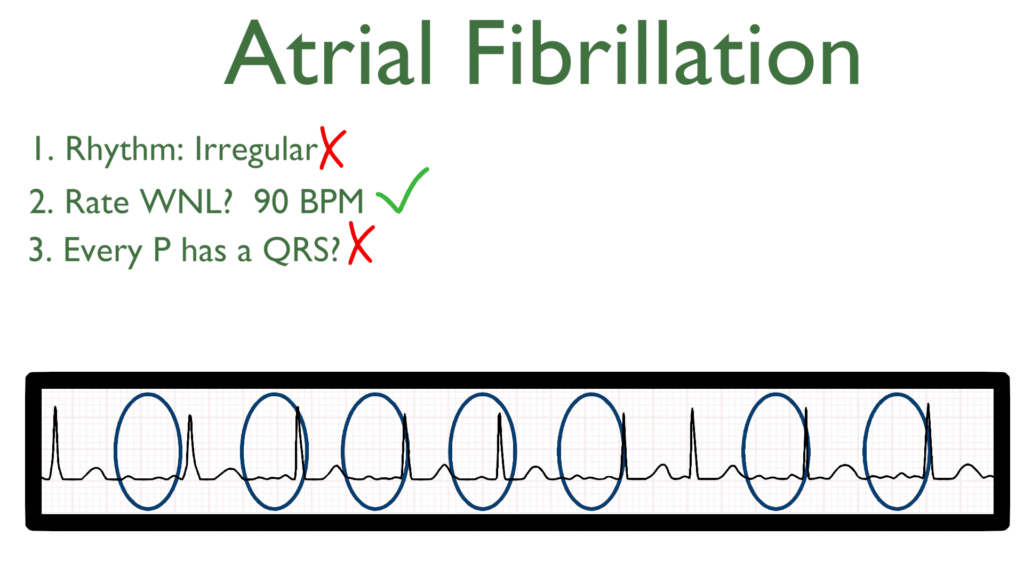
4. Assess the P waves and PR interval.
The PRI will be immeasurable due to the amount of P waves and the nature of ventricular contraction.
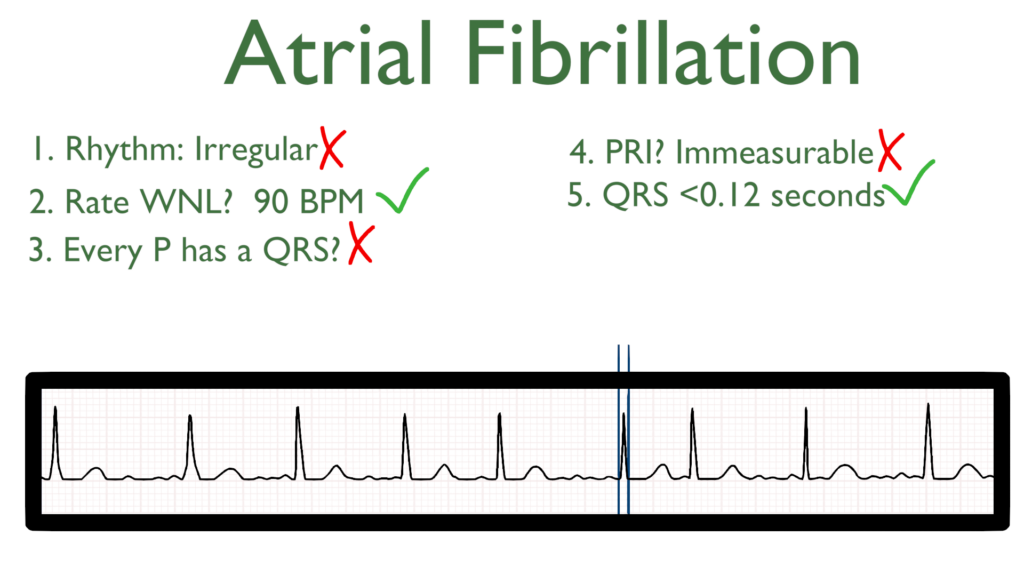
5. Assess the QRS.
The QRS will be within normal limits.
The QRS should be between 0.06 seconds to 0.12 seconds.
Better yet, QRS should be between 1.5 to 3 small boxes.
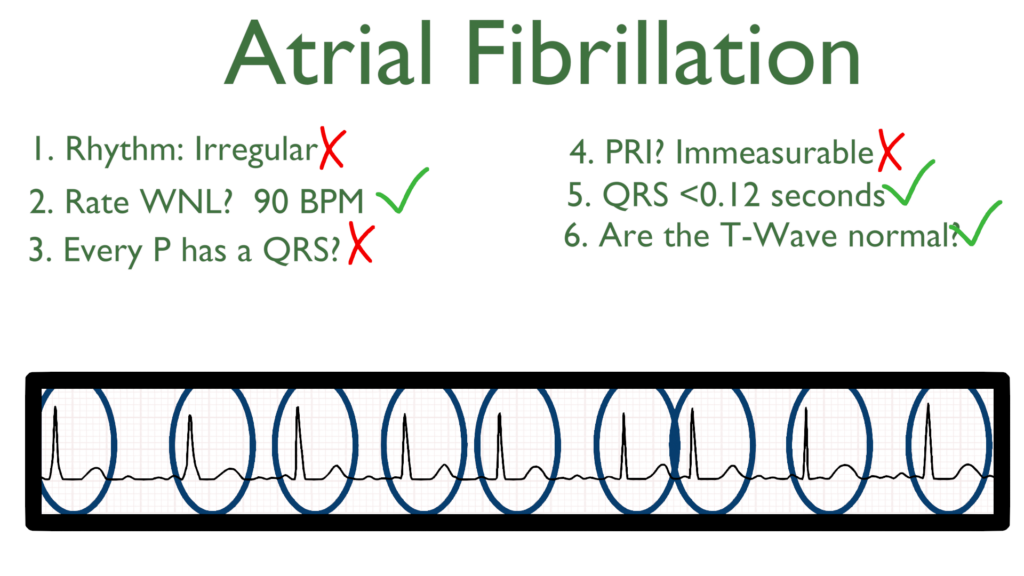
6. Assess the T waves.
T waves should deflect in the positive direction with no ST-Elevation or ST-Depression.
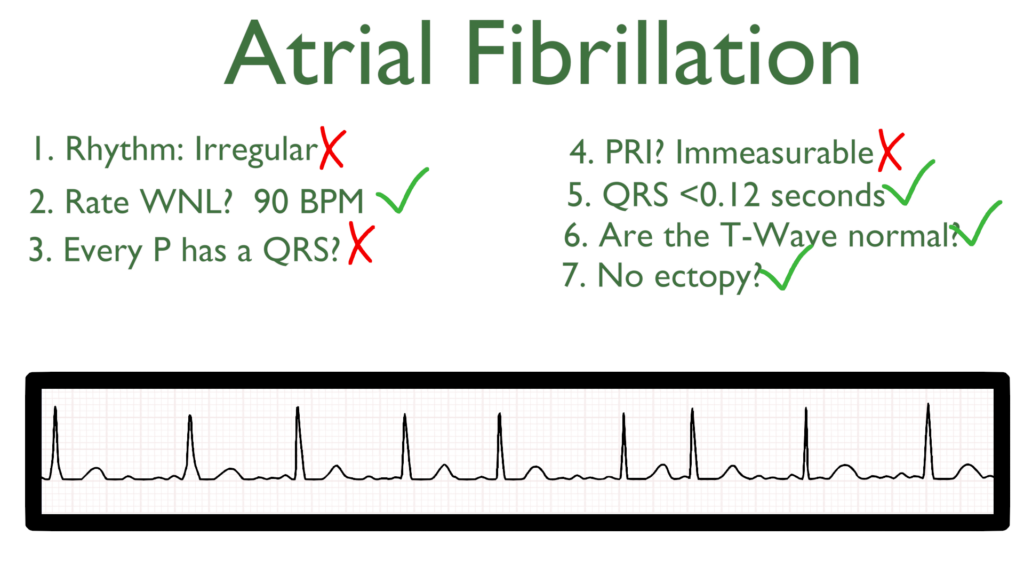
7. Assess for Ectopy.
As you can see on this 6 second strip there are no ectopic beats. This is to say there are no PVC’s or PAC’s present.
Treatments for A Fib
Stable
i.e. asymptomatic and normotensive
In a stable condition patient may be given oral or I.V. medications to treat the dysrhythmia.
Beta blockers such as atenolol, metoprolol, propranolol, or labetalol.
Calcium channel blockers such as diltiazem, nifedipine, amlodipine, or nicardipine
Unstable
i.e. hypotensive with or without symptoms
Patients in an unstable condition may be treated with:
Synchronized cardioversion
Catheter ablation
I.V. medications (at times these medications are given as a push and then started as a continuous drip)
Beta blockers such as atenolol, metoprolol, propranolol, or labetalol.
Calcium channel blockers such as diltiazem, nifedipine, amlodipine, or nicardipine
Special Considerations
Stroke Risk
Within both atria there is what is called the atrial appendage, for the sake of A Fib we will directly talk about the Left Atrial Appendage (LAA). This little flap off of the side of the atria is there as an atrial pressure regulator which will also secrete pressure regulating hormones.
When it comes to A Fib, blood will not flow normally in an out of the LAA, but will pool within this little piece of the atria. When blood pools anywhere in the body clots may form in the blood that is not moving.
During A Fib when blood pools in the LAA clots will form which can then be pumped out of the LAA during a strong enough atrial contraction, which can then lead to an ischemic stroke.
The LAA is regarded as the most common source of clot formation where estimates place the LAA as the clot source of up to 90% of strokes caused by A fib (Sakellaridis et. al., 2014).
Since the LAA is the most common source of clot formation in stroke patients will usually be place on an anticoagulant. Anticoagulant’s commonly used are warfarin, eliquis, xarelto, and sometimes aspirin.
Rapid Ventricular Response (RVR)
This is to say that as impulses in the atria are being generated often, many of these are passing through the AV node causing the ventricles to contract as well creating a high heart rate.
With RVR patient assessment will be exceedingly important as RVR has the potential to create an unstable patient condition caused by a decrease in cardiac output. Monitor patient symptoms and vitals closely in patients with RVR.
References
Sakellaridis, T., Argiriou, M., Charitos, C., Tsakiridis, K., Zarogoulidis, P., Katsikogiannis, N., Kougioumtzi, I., Machairiotis, N., Tsiouda, T., Arikas, S., Mpakas, A., Beleveslis, T., Koletas, A., & Zarogoulidis, K. (2014). Left atrial appendage exclusion-Where do we stand?. Journal of thoracic disease, 6 Suppl 1(Suppl 1), S70–S77. https://doi.org/10.3978/j.issn.2072-1439.2013.10.24
