Video
Stay tuned for the video!
Definition
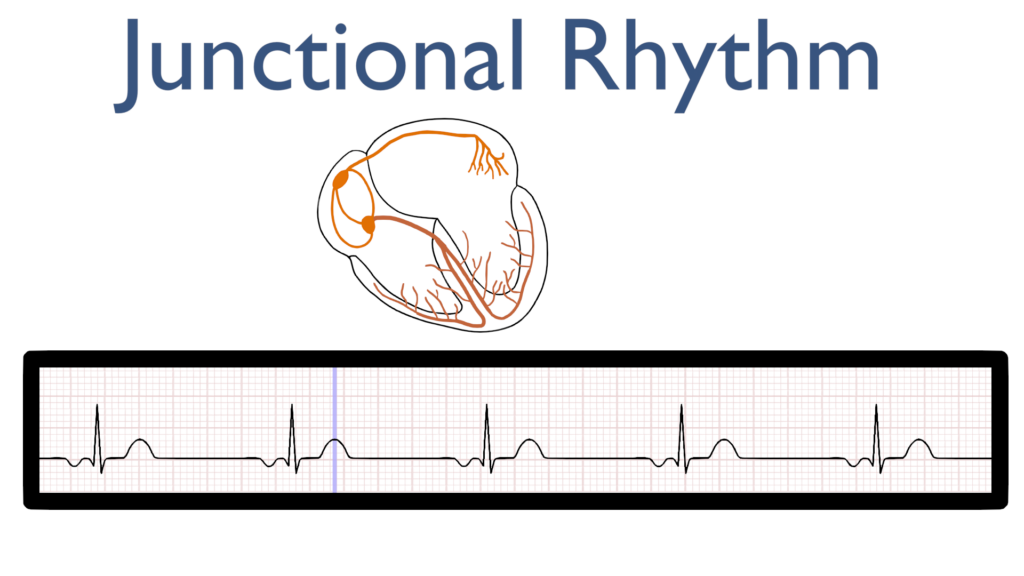
First, consider the definition of “junction.” Junction is defined as a point where two or more things are joined.
When you think of a junctional rhythm, think of a rhythm originating where the atria and ventricles are joined i.e. the AV node.
Junctional rhythms happen when either the SA node has no pulse originating from it leaving impulse generation to the AV node or when the AV node is firing with a stronger impulse than the SA node.
The key here is understanding the the SA node is not working appropriately and that the AV node has completely taken over as the “pacemaker” of the heart.
*Remember, the AV node is capable of sustaining heart rates between 40-60 beats per minute*
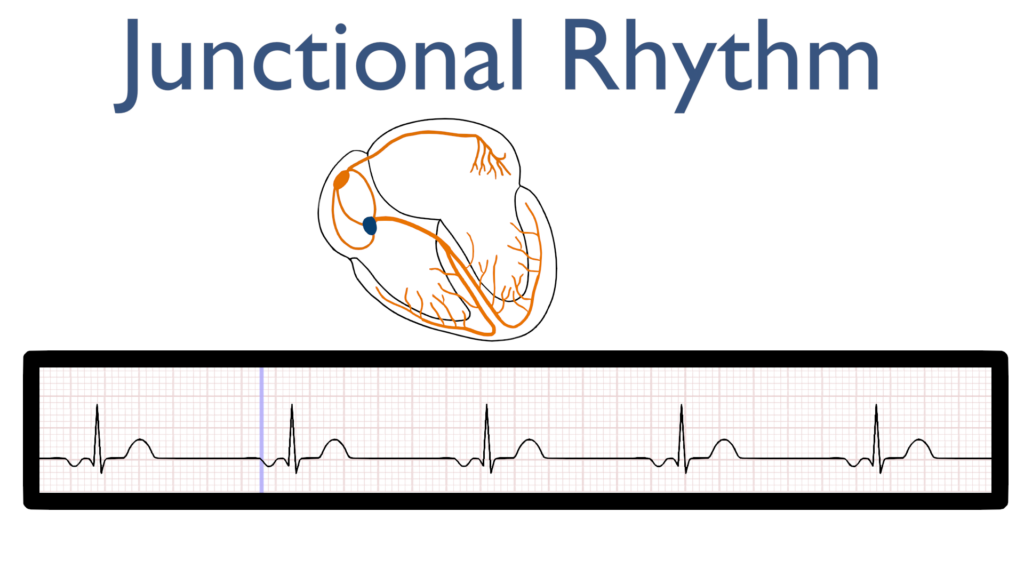
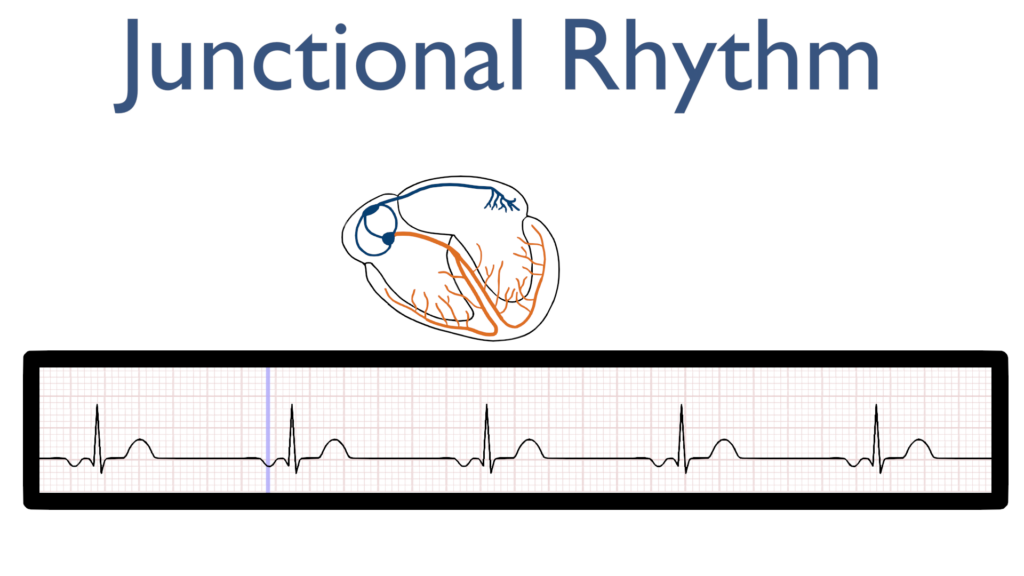
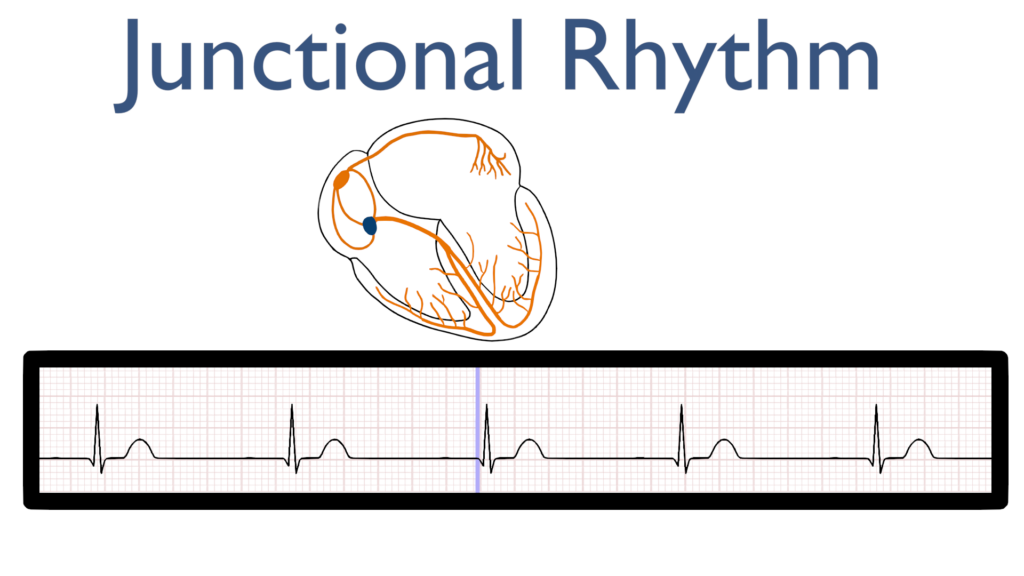
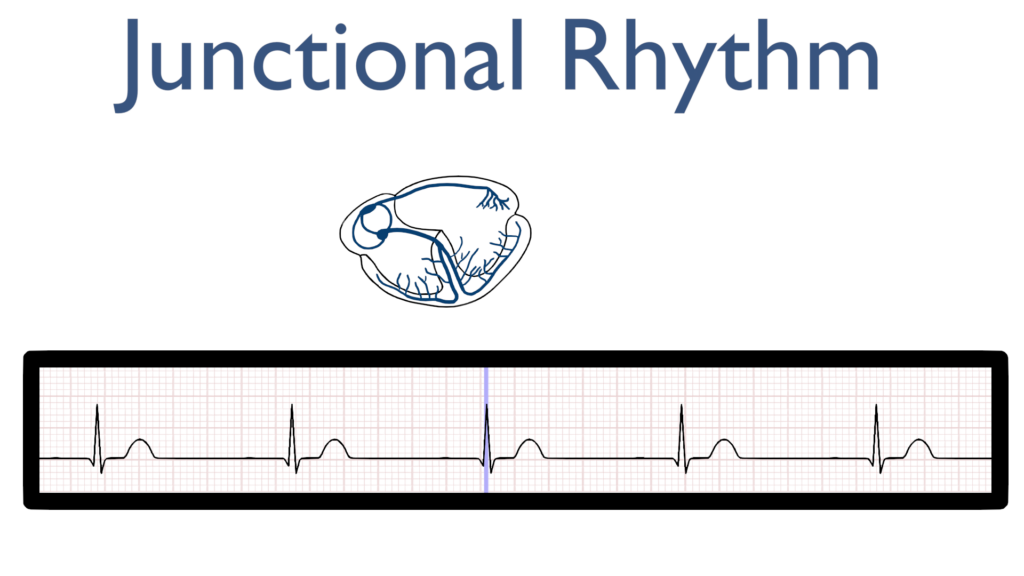
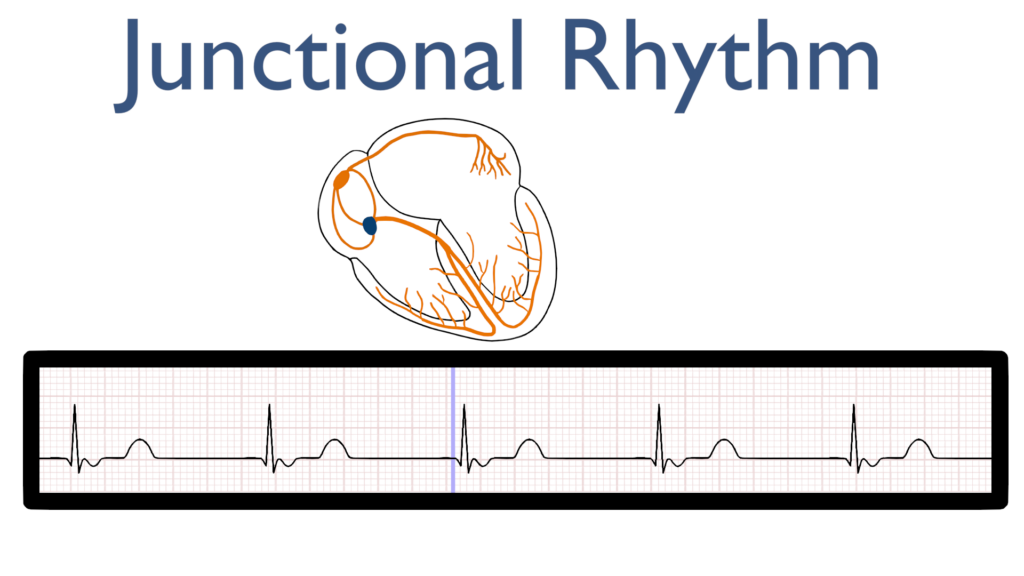
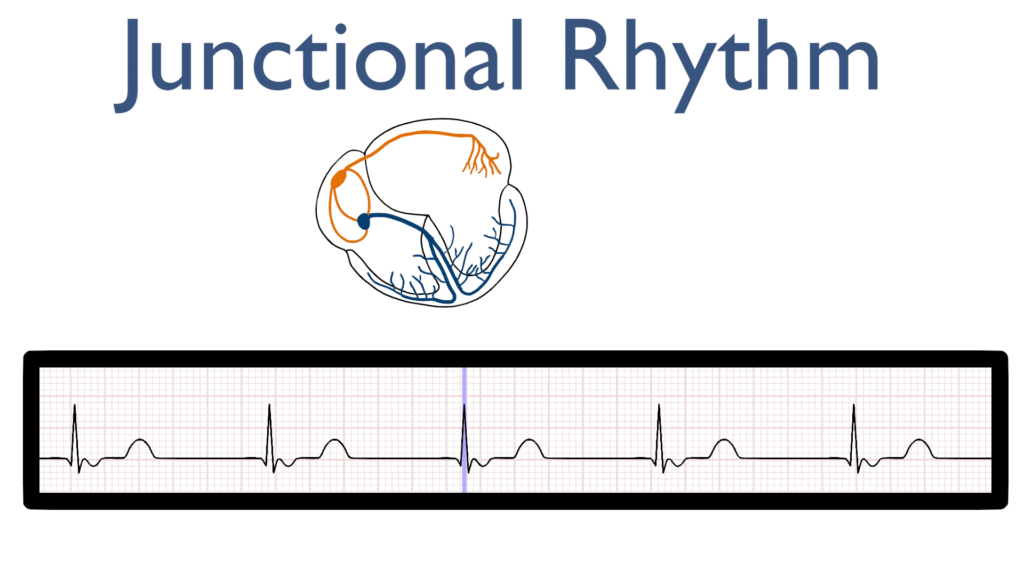
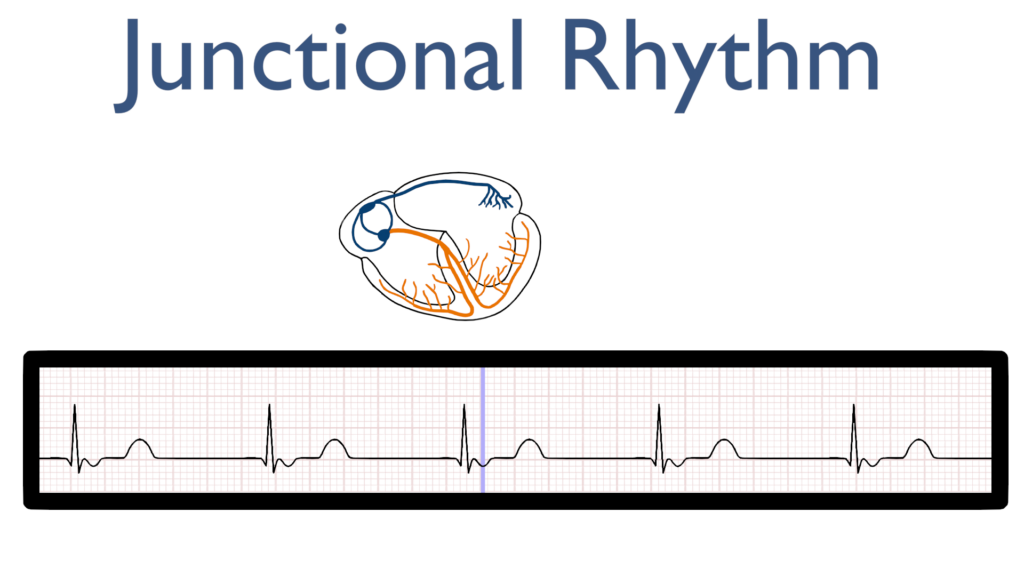
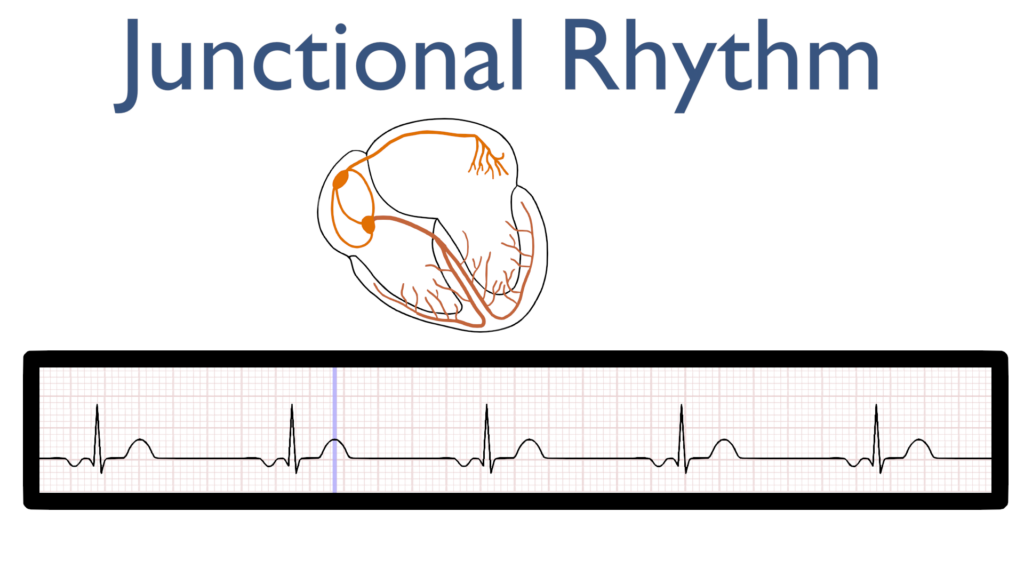
What’s happening in the heart
Atrial Contraction
First, the impulse originates in the AV node and then travels up throughout the atria.
This is seen as an P-wave that is deflecting in the negative direction on most leads. Often referred to as a retrograde P-wave.
Another way of considering the P-wave deflection for junctional rhythms is that the P-wave deflection should deflect in the opposite direction of the QRS.
To fully understand why this impulse is a downward deflection consider back the 3-lead article where we discussed impulse direction of travel relative to the electrode picking it up.
It is also good to note that the P wave may be buried within the QRS signal or may even appear between the QRS and the T-wave.
Now, knowing where the impulse is originating consider why we may see atria depolarization at three different times.
P-wave before QRS
P-wave buried in QRS
P-wave after qrs
Ventricular Contraction and Repolarization
Next, just as with a normal sinus rhythm we should see a typical QRS and T-wave.
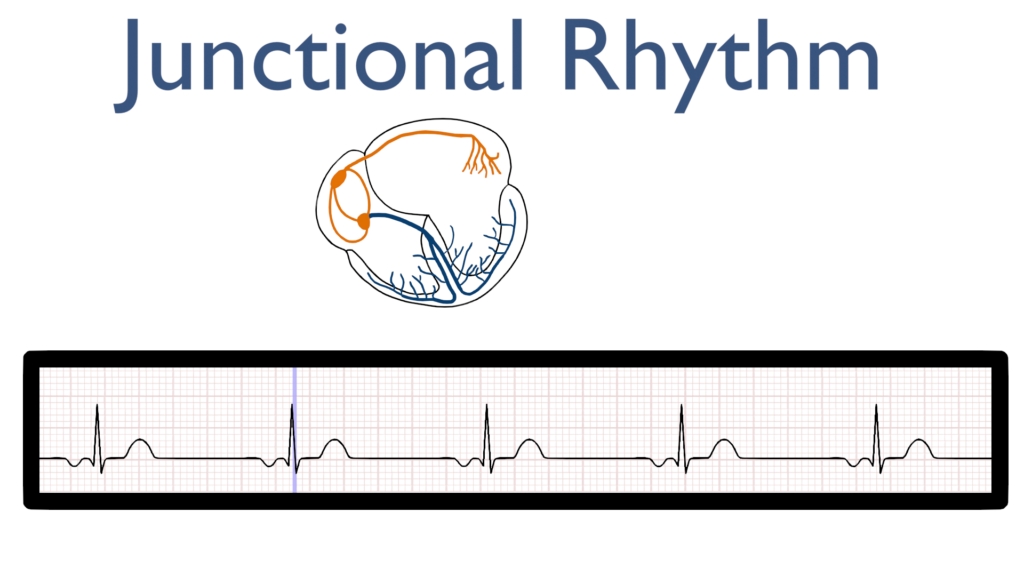
Seven steps of rhythm interpretation
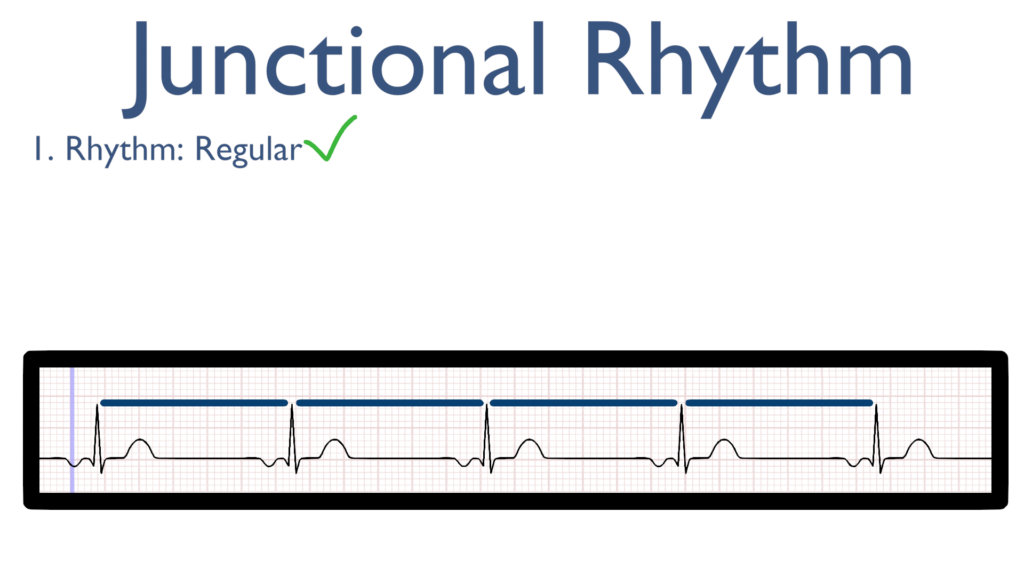
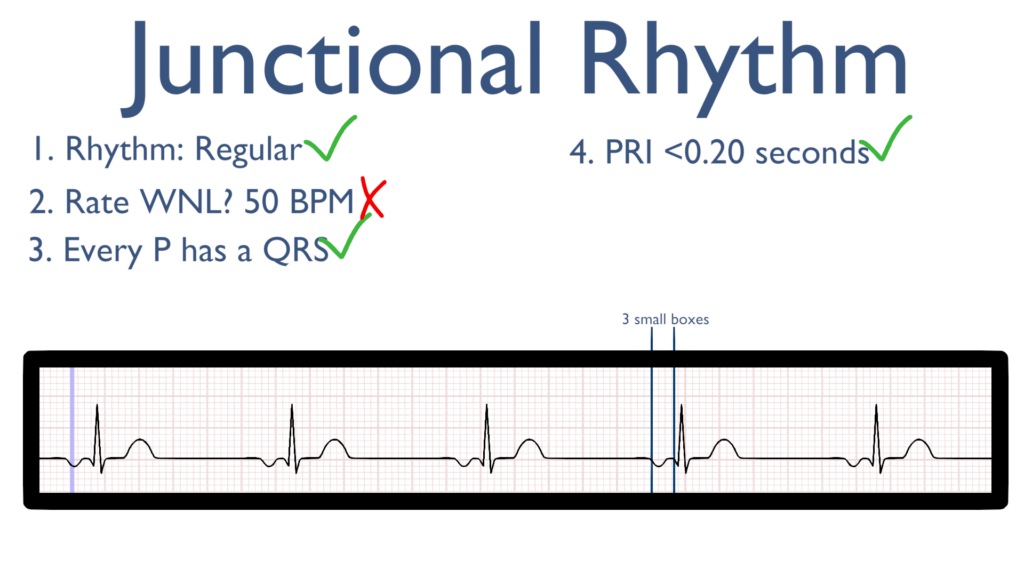
1. Assess the rhythm.
First, the rhythm should be regular. This can be identified by regularly spaced R waves.
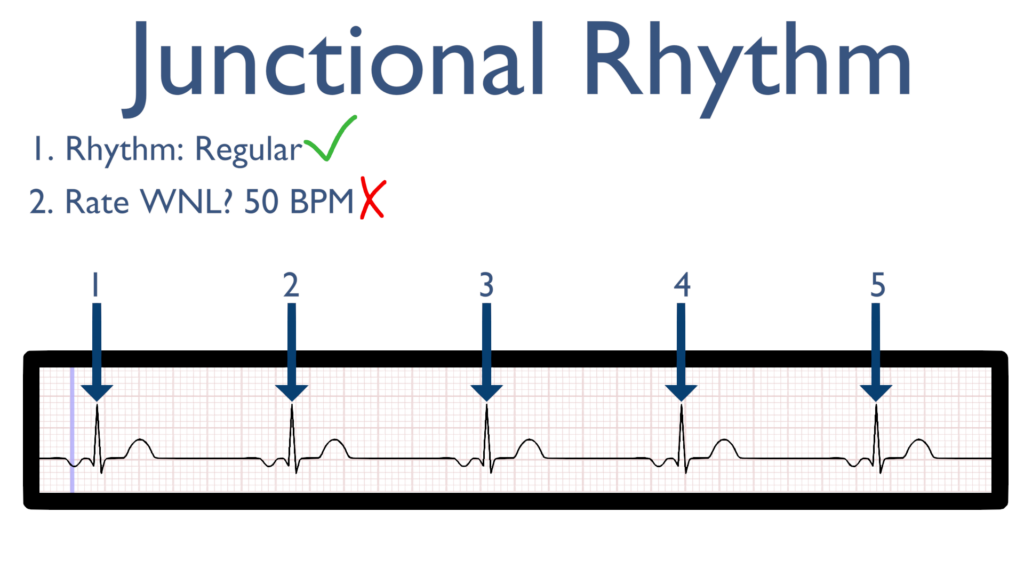
2. Assess the rate.
Next, when assessing the rate you will find with a standard junctional rhythm it will be between 40 and 60.
*This will be the differing variable between junctional, accelerated junctional, and junctional tachycardia.*
3. Assess atrial and ventricular rates.
Next, we will see a QRS directly after every P wave.
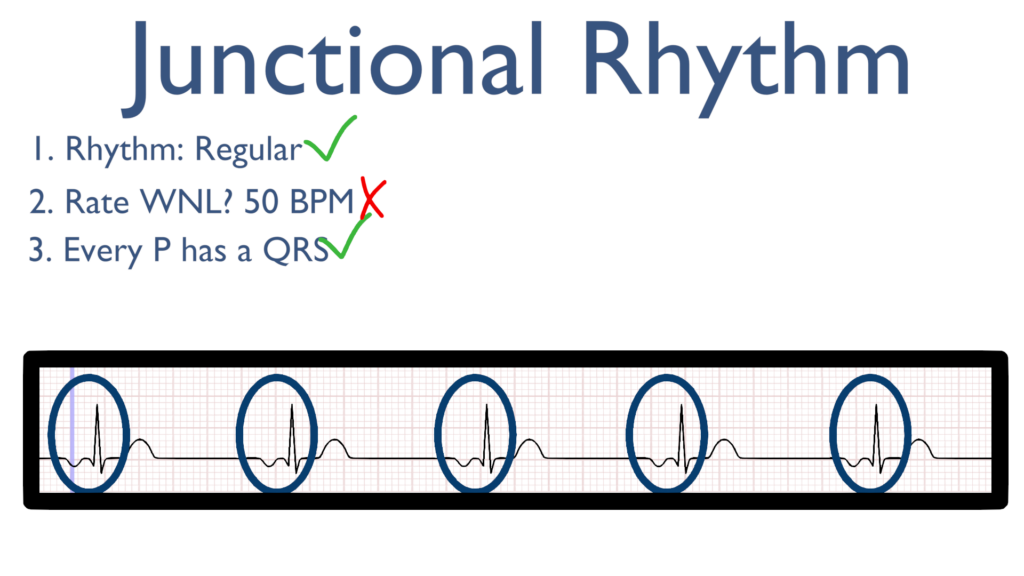
4. Assess the P waves and PR interval.
Now take a look at the P waves. With junctional rhythms P waves will deflect downward (or better yet opposite of the QRS deflection).
The PRI (if present) will be less than 0.20 seconds (4 small boxes).
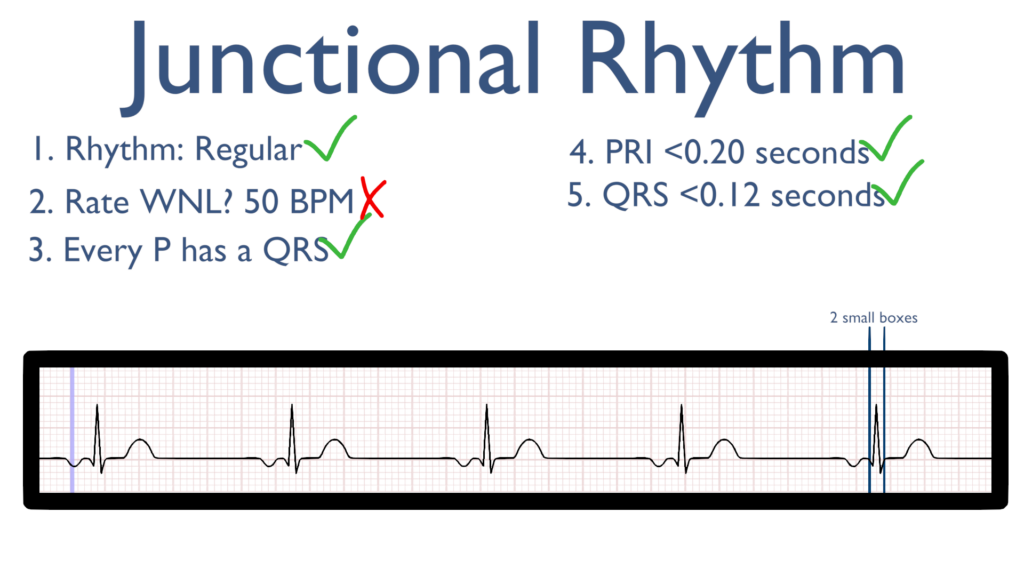
5. Assess the QRS.
Here take a look at the QRS complex.
The QRS should be normal which will be considered <0.12 seconds (3 small boxes).
6. Assess the T waves.
T waves should deflect in the positive direction with no ST-Elevation or ST-Depression.
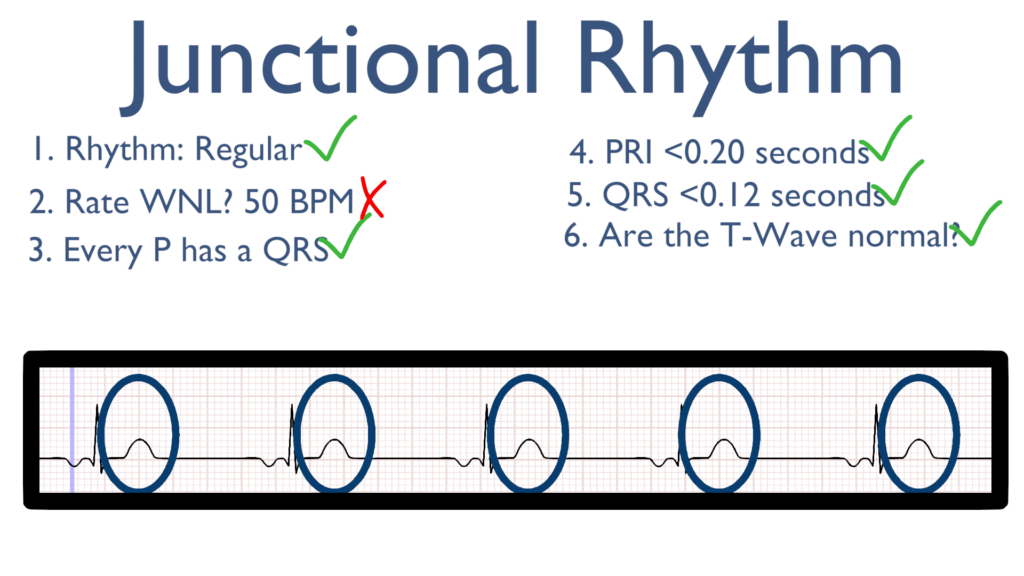
7. Assess for Ectopy.
As you can see on this 6 second strip there are no ectopic beats. This is to say there are no PVC’s or PAC’s present.
Treatments for
Stable
i.e. asymptomatic and normotensive
Unstable
i.e. hypotensive with or without symptoms
Pacing and pacemaker placement may be considered.
Atropine
Digoxin reversal agents