Video
Below is a quick video snap shot of this article.
Definition
First, think of what “supra ventricular” means. Supra means above, so supraventricular tachycardia quite literally means above the ventricles tachycardia.
Supraventricular Tachycardia, more commonly known as SVT, is a tachy heart rhythm that originates at or above the AV node with no defining characteristics of other tachy dysrhythmias.
SVT is actually more of a categorization of tachy dysrhythmias than it is an actual tachy rhythm. This is to say that with SVT we know that the rate is quite fast, greater than 100 bpm but more often even greater than 160 bpm, yet we can not identify any characteristics that would lead us to believe it is a more specific rhythm such as A-Fib or A-Flutter.
The category of SVT actually contains all of our tachy dysrhythmias such as Sinus Tachycardia, Atrial Fibrillation, Atrial Flutter, junctional tachycardia, and even multifocal atrial tachycardia. Since all of these dysrhythmias originate above or at the AV node and are tachy they can be classified as and SVT rhythm.
When we say that someone is in SVT we are saying that it is a tachy rhythm that originates above the AV node but we cannot identify which specific rhythm it is. A good way to think of this is that SVT is not an actual rhythm but is the lack of identification of an actual rhythm.
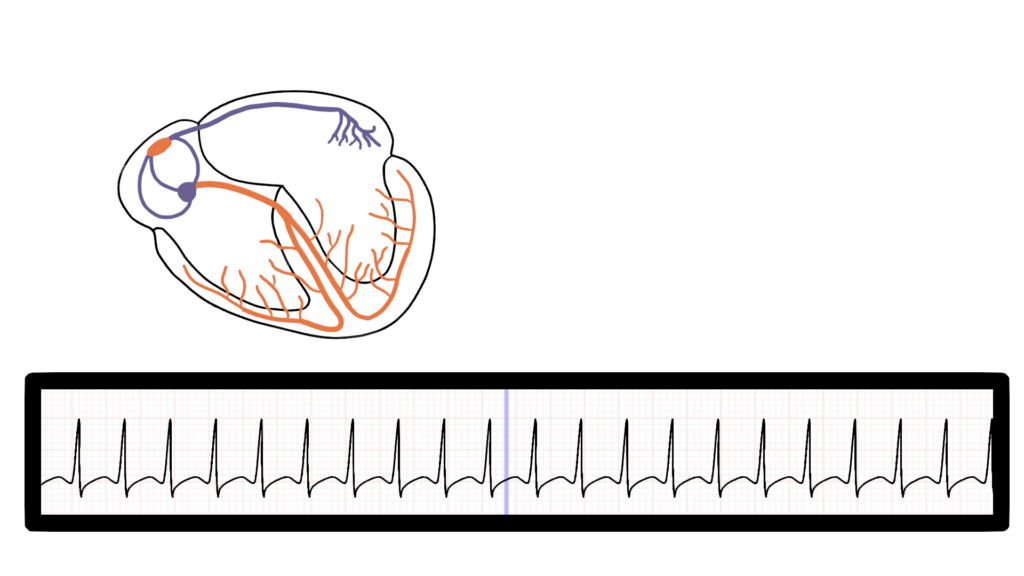
We generally can not identify which tachy dysrhythmia this is because of how fast the rate is. The ventricles are depolarizing so fast that on the ECG strip we have no discernible p-waves or t-waves. Essentially, we can only see QRS after QRS, and we can identify that the QRS is within normal limits. This means that the ventricles are depolarizing and repolarizing normally, which means that the ventricles are working appropriately.
What’s happening in the heart
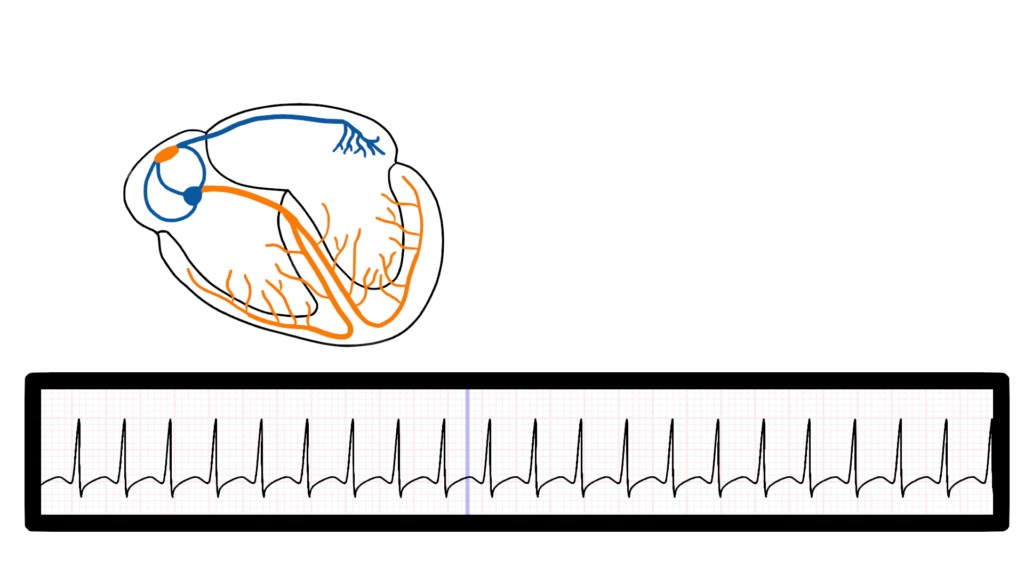
Atrial Contraction
When comes to SVT we know that the impulse is originating above the ventricles.
The impulse may originate in the SA node, or anywhere within the atrial as it does with A. Fib.
As you can see the P-waves overlap with the T-waves which makes it impossible to identify what the rhythm actually is.
Ventricular Contraction
Ventricular depolarization happens just as it does with a normal sinus rhythm, with a narrow complex.
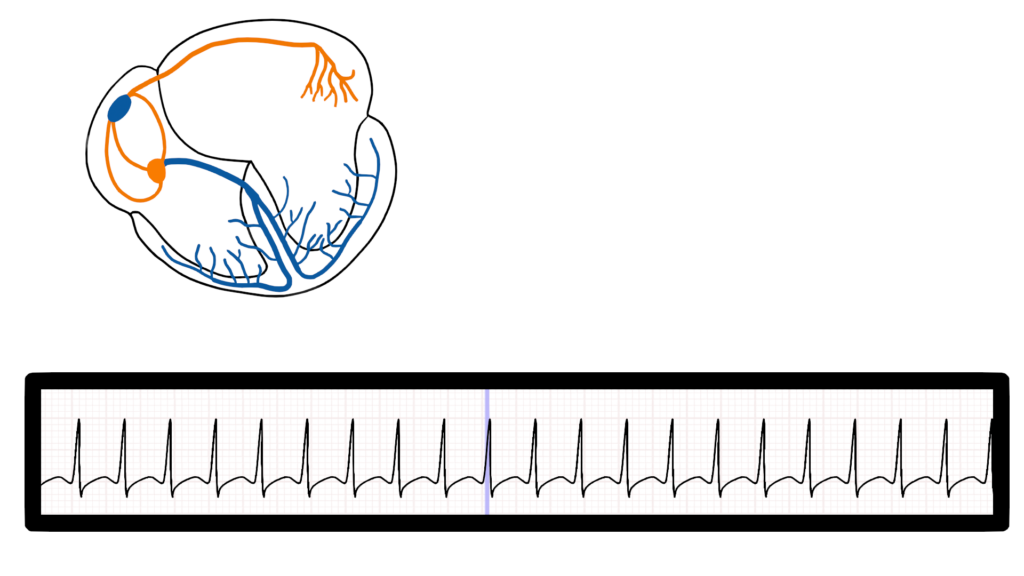
Ventricular Repolarization
The ventricles repolarize just as they do with a normal sinus rhythm.
Since the rate is so fast ventricular repolarization and atrial depolarization take place almost simultaneously. This is seen as an overlap between the P-waves and the T-waves.
Since the P-waves overlap with the T-waves we cannot identify which rhythm this is, this is why we categorize this rhythm as SVT.
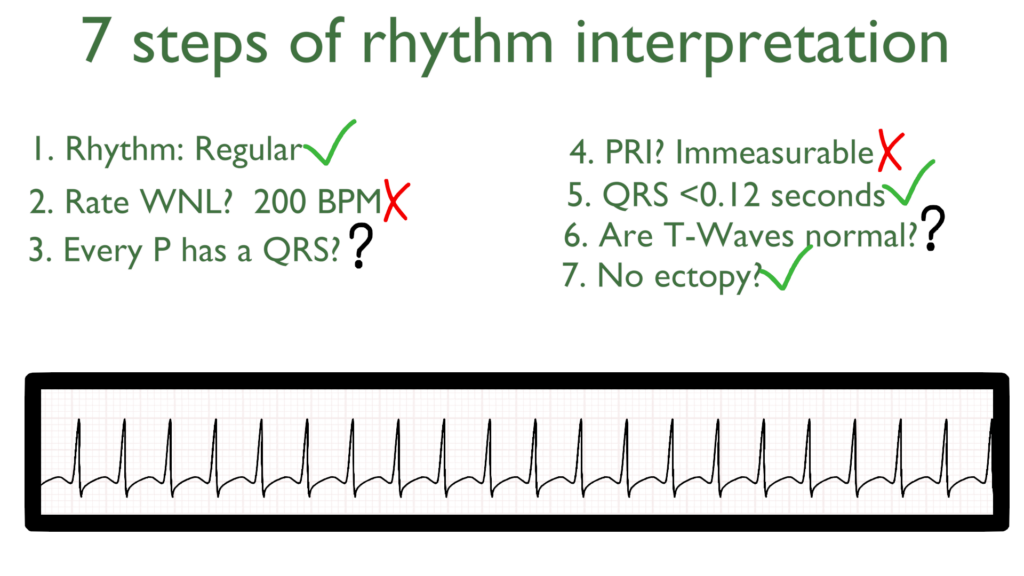
Seven steps of rhythm interpretation
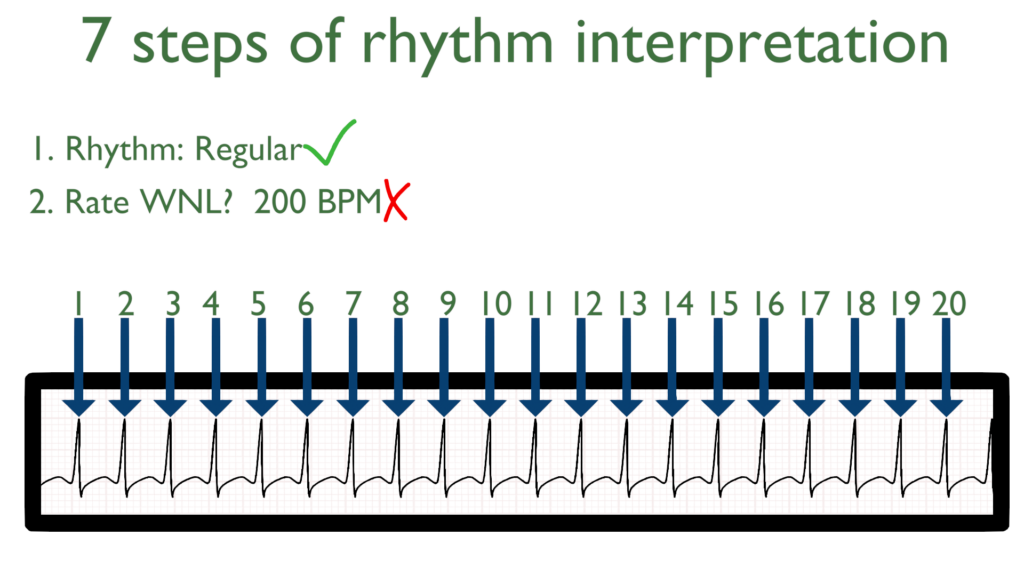
1. Assess the rhythm.
First, the rhythm will mostly likely look regular due to how fast it is.
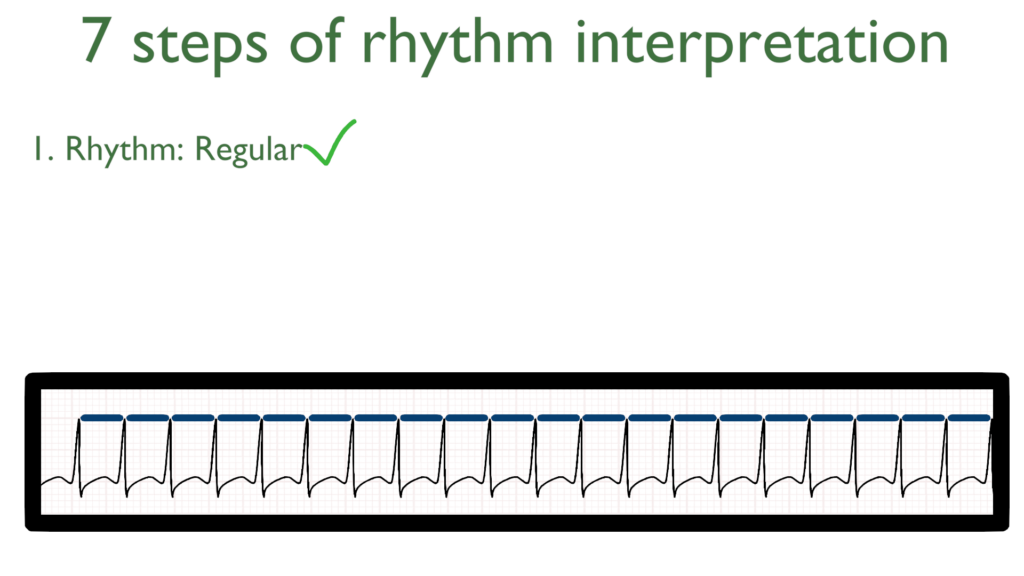
2. Assess the rate.
Next, when assessing the rate you will find that the rate is extremely fast.
For SVT it is most often greater than 160 BPM and even often greater than 200 BPM.
3. Assess atrial and ventricular rates.
Assessing if the atrial and ventricular rates are equal will be immeasurable here due to the overlapping P and T waves.
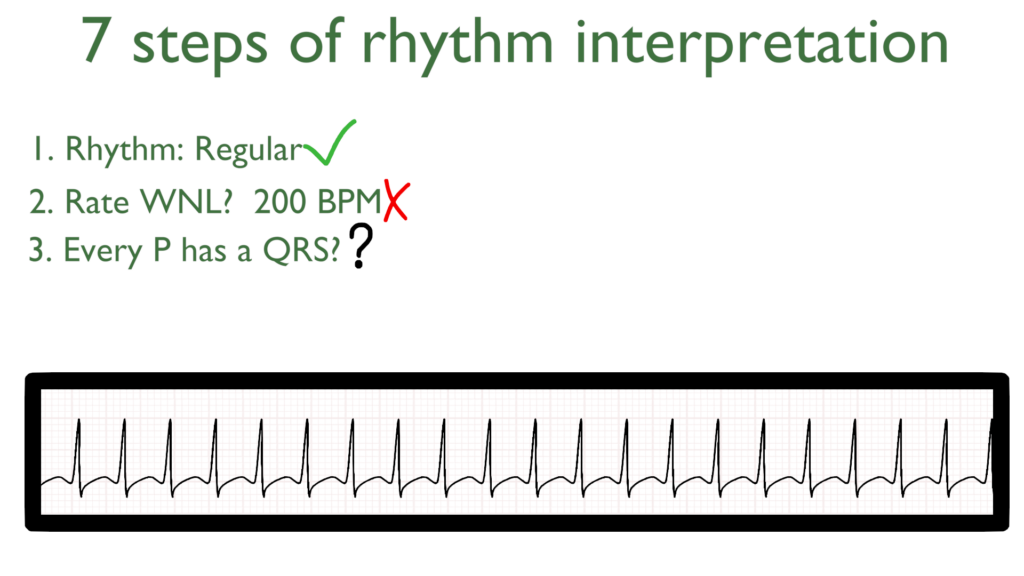
4. Assess the P waves and PR interval.
With SVT the PRI will be immeasurable due to being unable to identify the beginning of the P-wave.
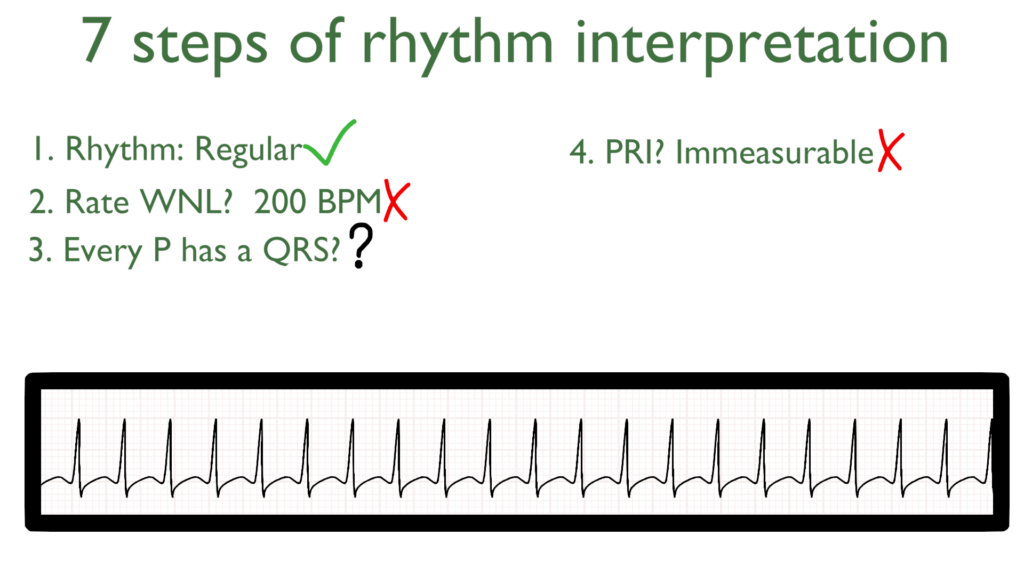
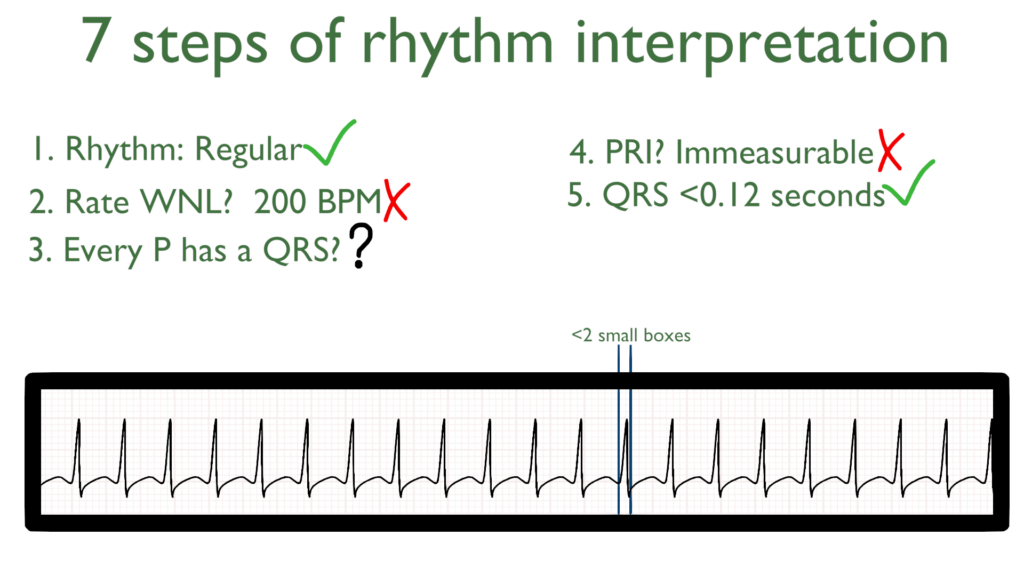
5. Assess the QRS.
Here take a look at the QRS complex. With SVT the QRS will be narrow complex that is less than 0.12 seconds, or less than 3 small boxes.
6. Assess the T waves.
Just as the P-waves are immeasurable, the T-waves will be immeasurable as well.
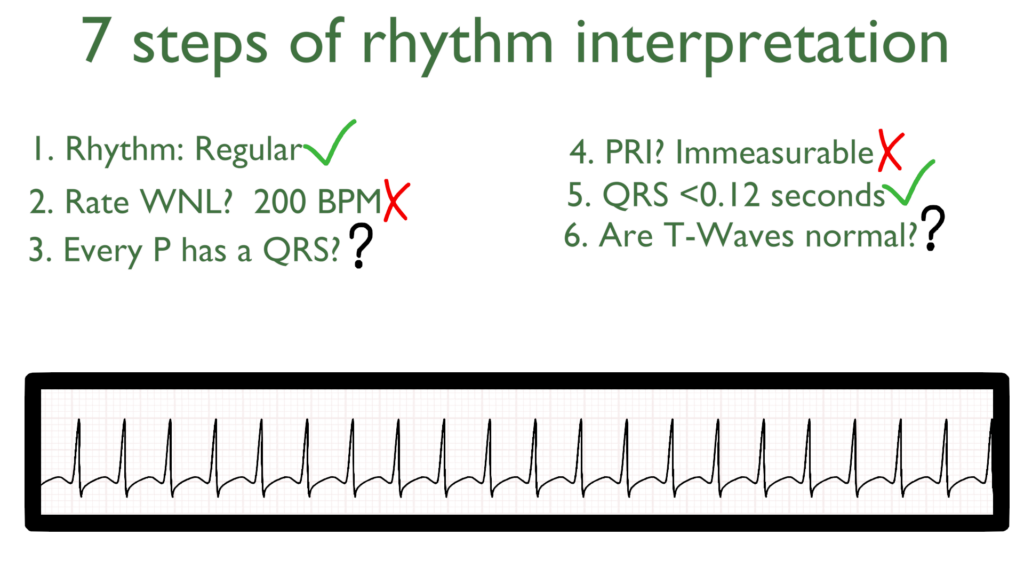
7. Assess for Ectopy.
As you can see on this 6 second strip there are no ectopic beats. This is to say there are no PVC’s or PAC’s present.
Paroxysmal SVT
SVT is most often caused by medications, electrolyte abnormalities, caffeine, alcohol, physical or emotional stress, or cigarette smoking.
Paroxysmal SVT is a sudden occurrence or sudden recurrence of SVT with no known causes, such as those stated above.
With Paroxysmal SVT the rate is generally greater than 160bpm and can even be over 200 bpm.
Paroxysmal SVT may come and go without the patient even knowing it is happening. There may be short bursts where there are just 10 beats or it may come and stay until medical interventions are completed.
Treatments for SVT
Treatments for SVT focus on slowing the dysrhythmia down to visualize the underlying rhythm, or converting this dysrhythmia back to a normal sinus rhythm via chemical or mechanical cardioversion.
Stable
i.e. asymptomatic and normotensive
Prior to treatment with medications Vagal Maneuvers may be considered.
Vagal Maneuvers
Carotid sinus massage
Valsalva maneuver (bearing down or blowing through a straw / syringe)
Diving reflex (ice cold water to the face while holding ones breath)
Medications:
Adenosine
Unstable
i.e. hypotensive with or without symptoms
Recurrent SVT
